After your operation you will be transferred to a ward area where you are closely observed. This area has a higher nursing staff ratio to enable close monitoring for the first 48 hours after your operation. The operation will take 4 to 10 hours depending on whether you are having one or two flaps. You will probably feel drowsy until the next day so it is advisable for your next of kin to telephone the ward before visiting.
When you wake up you will have a urinary catheter, a drain in each reconstructed breast and a drain in the abdominal donor site.
After your operation I encourage you to get out of bed as soon as possible. If you return to the ward early enough that may even be on the same day. This helps to open your airways up following the long anaesthetic. On the first day after the operation you will sit out of bed and do some short walks. We aim to remove the catheter later the same day.
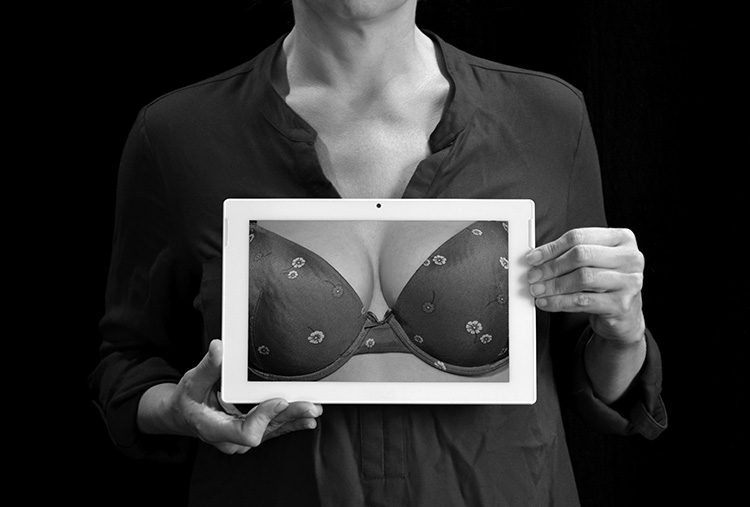
You will have some tape dressings on the wounds and will put the bra on before getting out of bed to support the reconstruction. You will have a warming blanket (bair hugger) on for the first 24 hours after the operation. It is important to keep the area warm to maintain a good blood supply to the flap.
Your abdominal wound may feel tight following surgery. To improve comfort you can sit with you hips bent.
The nursing staff will make regular observations including blood pressure, temperature, flap observations, drip monitoring and oxygen monitoring. The flap is closely observed during the first 48 hours to ensure that any problems with the blood flow are picked up early and dealt with in a timely fashion. If any problems with blood flow to the flap or other problems such as bleeding occur it would be necessary to return you to theatre to investigate the cause.
Do not be alarmed by the number of drips and drains you have when you first return from theatre, this is quite normal for this type of surgery.
IV Drip
This is used to give you fluids and keep you hydrated whilst in theatre and immediately afterwards when you are too drowsy to drink. It can also be used to give medication if required. Fluids are normally discontinued once you are drinking good volumes.
Catheter
This will be inserted once you are asleep and allows you to pass urine without getting out of bed. As soon as you are up and about this will be removed.
Many women have anxiety about the catheter however it generally causes very little discomfort and is easy to remove.
Drains
You will have one drain at the site of the reconstructed breast and are likely to have one or two in the abdomen as well. These are removed before you are discharged.
Oxygen
You will have oxygen administered initially via a mask then through small tubes that sit in the nostrils. This is required until your oxygen levels are back to normal.
Compression boots and stockings
You will wear anti-thrombus stocking throughout you admission and for 6 weeks after discharge.
In addition to this you will have inflatable cuff on the calves during your operation and for 24 hours afterwards. These inflate and deflate in a cycle and gently massage the calves to help your circulation to continue to flow well whilst you are less mobile.
During your hospital stay our physiotherapists will see you on several occasions. The aims of physiotherapy following breast reconstruction are to prevent you developing breathing problems such as chest infections, to help get you mobile again, to help you regain strength and movement in your shoulder and arm and to advise you on returning to your normal daily activities.
Your physiotherapist will show you some exercises you can do for your lower body to prevent stiffness and aching in your joints. Moving your feet and ankles helps your circulation and relieves pressure on your heals.
On the first post-operative day you will be helped to sit out, stand up and walk short distances. As you start moving there will be a little soreness and pulling at the wounds but do not worry they will not split. You may find it difficult to stand up straight initially due to pressure on your donor site but this area becomes more comfortable over the next few days. You will increase this distance you walk every day and aim to do stairs on the day of discharge.
Following breast reconstruction there is a small risk you will develop a stiff shoulder. This is because the surgery is in close proximity to the shoulder joint and you will inevitably be a bit reluctant to move your arm. In immediate reconstruction you may also have had surgery to the axillary lymph nodes.
Your physiotherapist will advise and guide on which shoulder exercises to do and when. You should usually start these exercises the day after surgery. You will probably feel tightness, pulling and discomfort when you do the exercises. This is normal however if it is very painful please discuss this with your physiotherapist. What to Expect on Discharge
You will have all your dressings checked on the day of discharge, which is usually 3-5 days after surgery. At this stage you will still not be using the arm on the operated side for any lifting or carrying and you may still feel a little weak. You should have another adult at home with you for the first week after discharge. You will be seen again in the dressings clinic approximately one week following discharge.
It is normal to feel tired after major surgery so do not over exert yourself for the first few weeks at home. You may find simple tasks such as getting washed and dressed leave you feeling tired. Try to get plenty of rest and always balance periods of activity with periods of rest. Build up your stamina by going for a walk everyday, increasing the distance you walk each time. Continue to do the shoulder exercises that you have been given in hospital and begin any new exercises as directed. You should continue the exercises until twelve weeks after your operation.
Scar Management
Scar tissue is vital to the healing process however scars can tighten, limit movements and become uncomfortable. Massage helps to encourage the scar tissue to form in the correct lines and make a more functional rather than restrictive scar. Massage also makes the scar less sensitive and prevents adhesions.
To massage apply a small amount of simple un-perfumed moisturizing cream to the scar. Use the thumb or index finger to massage in small circular motion along the scar. Use a firm pressure and massage several times a day. Only start the massage once the wounds are fully healed (nurses will provide you with guidance on this).
Returning to Normal Activities
There are no strict rules for when you return to work, driving or sports and this will depend upon you as an individual, how you heal and the nature of your work or hobbies. I will give you guidance in the clinic, the following information gives you a generalized idea of what to expect.
Two weeks after your operation you can use the arm on the affected side for light activities eg lifting a full kettle or brushing your hair. Over the next 4 weeks you can build up the use of this arm by doing light household activities such as dusting and preparing light meals. At 6 weeks after the operation you should have returned to most normal daily activities such as carrying shopping and hovering. You will not however have normal energy levels until around 12 weeks post-op.
Return to Work
This will depend on the type of work you do. For office jobs or other non-physical work you can probably return at 6 weeks although you may find you tire easily and therefore it may be appropriate to negotiate reduced hours for the first couple of weeks. If your work is physical and involves heavy lifting you could return on light duties if possible at 8 weeks post-operatively but you should not do any heavy lifting until at least 12 weeks post-operatively. When you return to work you will need to gradually build up your strength so may benefit from a phased return.
Return to Driving
You should avoid driving for 4-6 weeks after surgery. You should not return to driving until you feel 100% alert and able to react in an emergency. You must have regained full shoulder movement before attempting to drive. You must always wear your seatbelt when in the car.
Return to Sport
Provided you have healed you can return to sports at 4 - 6 weeks but you should start with less vigorous activities and gradually build up your level of activity. You will be unfit and will need to build slowly. You should not participate in contact sports or raquet sports until 3 months after your surgery.